| A refractive surgeon has to wear many
hats
with patient counselor and surgeon being just two. When a
patient presents with an interest in refractive surgery
because his eyes feel too dry and gritty to tolerate contact
lenses, your first reaction might be to treat him for dry eye
before doing his Lasik. It's been my experience that it might
be better to step back and put on the hat of the
diagnostician, because the patient's problem may not be due to
dry eye, but rather a different condition altogether. In this
article, I'll explain how I get to the root of the
problem.
The
Diagnostic Pyramid
In
an effort to properly diagnose and subsequently treat
refractive surgery patients with tear-film abnormalities, I
codified my thought process into a decision pyramid. The
diagnosis methods begin at the top with the more
straightforward, routinely used ones and eventually lead
downward toward the more involved methods for patients whose
problems are harder to pinpoint. I try to turn the subjective
symptoms into an objective diagnosis, thus determining whether
a patient has dry eye or another condition. If a patient is
pigeonholed as having dry eye when he actually is suffering
from something else, he could be relegated to years of using
the wrong drops without relief.
. First level: Routine
tests. After listening to the patient describe his symptoms,
the first step toward determining their cause consists of
in-office tests such as Schirmer's tear test, fluorescein,
rose bengal and lissamine green staining, and tear-film
clearance and breakup time.
You
can also gather important information by examining the tear
film at the slit lamp with the room light dimmed. You will see
the tear lake and may see excessive tear splashing in the
ocular fornix, which will mean a deficiency in the oil layer
in the tear film. In this case, the patient may not have
aqueous-deficient dry eye, and instead may be suffering from
meibomitis. Artificial tears won't solve the problem. You can
instead advise lid scrubs, warm compresses or oral
doxycycline. A liposomal spray may be helpful in such
conditions.
Also,
find out if the symptoms get worse or better during the day.
If they're worse in the morning, it's probably meibomitis, not
dry eye. This is because as the day progresses the eye washes
the toxic tears away. If it were dry eye, however, it would be
the opposite: The eyes would be comfortable in the morning
after having had the lids closed all night, but then would
become drier during the day as they remain open. If the
patient has itching, this is a key sign of allergy; obviously,
bulbar edema and papillae in the upper lid clinch the
diagnosis.
. Second level:
Tear-film analysis. If you're still not certain what is
causing a Lasik patient's complaints of dryness and grittiness
after performing the usual in-office tests, you can perform
tear-film analysis and measure lactoferrin and IgE levels and
tear osmolarity. If it is dry eye, a lactoferrin microassay
with a device such as the Corneal Science Tear Profile
Analyzer (Touch Scientific, Raleigh, N.C.) will determine
whether it is aqueous-deficient dry eye (lactoferrin levels
below 0.9 mg/ml) or evaporative dry eye (lactoferrin levels
greater than 1.8 mg/ml). IgE levels will indicate ocular
allergies, and if they're high, the patient will need
anti-allergy medication, rather than artificial tears. In the
near future, gram negative and gram positive testing will also
be possible with this equipment.
This
testing can be a great help in determining the appropriate
treatment. For example, say a patient has meibomitis, but she
is diagnosed as having dry eye. When the artificial tears
don't work, the clinician will naturally proceed to punctal
plugs-just the opposite of what the patient needs. Now,
instead of having open puncta to allow the toxic tears to flow
away from the ocular surface, the toxins will stay there and
could cause surface damage.
The
cost of the machine ranges from $12,000 to $13,000. I have
used this system and believe it has the potential to specify
where in the dry-eye disease spectrum the patient lies. Though
the device's cost can be prohibitive, some practices get
around the expense by sending their patients' lactoferrin
samples to a central hub (usually a hospital or large practice
with the machine) for testing.
.
Third level: Tissue sampling. Brush and impression cytology
can show the stages of ocular surface involvement by
detecting keratinization, changes in cell morphology, loss of
goblet cells and other indicators. This might help determine
the severity of the condition and plan a surgery such as a
stem cell graft with amniotic membrane transplantation.
Next
in terms of invasiveness come biopsies of the lacrimal and/or
salivary glands. These could be useful in Sjögren's syndrome,
in which inflammatory, degenerative and infiltrative changes
will be evident. They can also reveal a more serious systemic
disorder for which dry eye may have just been a presenting
symptom. Blood or serum tests might be necessary to confirm
this.
The
patient you're evaluating for Lasik or examining postop could
have classic dry eye, Lasik-induced dry eye or something else.
By eliminating any false diagnoses, you can begin to treat him
effectively.
Dr.
Gulani is chief of the cornea and external disease department
and director of refractive surgery at the University of
Florida, Jacksonville.
| Post-Lasik
Dry Eye |
If
a patient presents post-Lasik with complaints of
dryness, there's a good chance it's the temporary
post-Lasik condition that mimics dry eye. Among the
reasons we know of for this condition is the
neurotrophic keratitis identified by Rockville Center,
N.Y., surgeon Eric Donnenfeld and others. They've
pointed out that making the corneal flap in Lasik,
especially if the hinge is superiorly located, can sever
the corneal nerves, resulting in a temporary
neurotrophic keratitis.
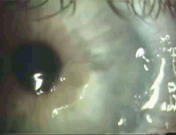
A
dry spot and yellow/orange iron deposits in a patient
with post-Lasik dry eye.
Another
important reason, I believe, for dry eye post-Lasik is
the change in corneal curvature between the treated and
non-treated zones caused by the ablation. This creates
an abrupt change in corneal curvature. This change
results in the tear film having difficulty in properly
draping the cornea, thereby resulting in stagnation of
the tears with iron deposition forming a ring that very
much resembles the deposits we see in keratoconus, the
Stocker's line in pterygium and the Ferry's line
associated with a filtering bleb in trabeculectomy. I
refer to this as the pseudo-Fleischer's ring, and it
points toward the cause of dry eye in the
patient.
With
post-Lasik dry eye emerging as the most common
complication of the procedure, we have to take it very
seriously, and share our integrated approaches to
treating it. Only by doing this will we be able to
progress toward the "super vision" that Lasik may
someday provide
patients. |
|