Category: Keratoconus
What’s New in Keratoconus Treatment?
Moving Beyond Contact Lenses with Dr. Gulani’s Advanced Vision Correction Understanding Keratoconus: When the Cornea Becomes the Obstacle Keratoconus is a progressive corneal disease where the cornea weakens, thins, and bulges into a cone shape, severely distorting vision. While specialty contact lenses temporarily mask some of the irregularity, they do nothing to stabilize the cornea […]
Can Keratoconus Be Cured? Vision Correction Beyond Contact Lenses & Transplants
Dr. Gulani’s Keratoconus Vision Correction: Beyond Contact Lenses & Corneal Transplants Keratoconus is a progressive corneal disease where the cornea thins, weakens, and bulges into a cone shape, distorting vision. While specialty contact lenses like scleral and rigid gas permeable (RGP) lenses can help mask irregularities, they don’t stabilize the cornea or address the root […]
Correcting Cross-Linking Complications: Restore Vision from Corneal Scars
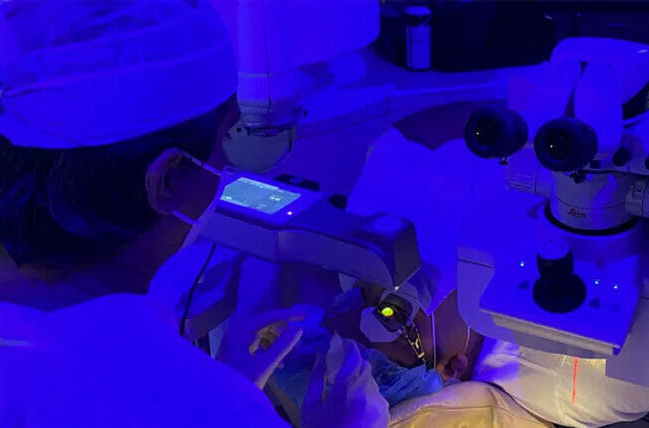
Keratoconus, a progressive corneal disorder that leads to thinning and irregular astigmatism, has long challenged ophthalmologists. While corneal cross-linking (CXL) is widely performed to halt the progression of keratoconus, it can sometimes result in blinding corneal scars, exacerbating visual impairment rather than improving it. LazrPlastique® at Gulani Vision Institute, to correct these vision-compromising corneal scars. […]
Beyond Crosslinking: Achieving Unaided Vision in Keratoconus Patients
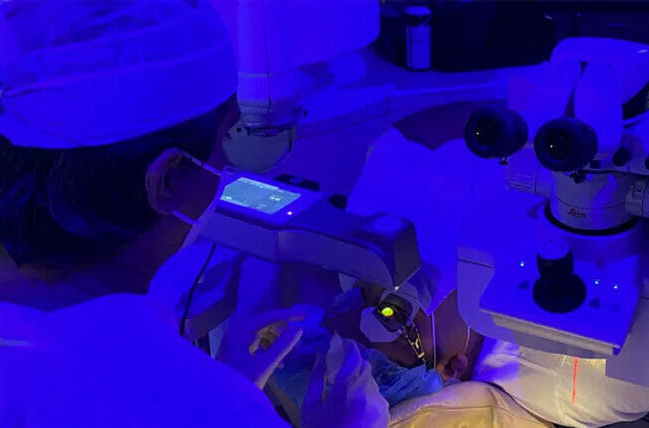
Correcting “Successful” Crosslinked KERATOCONUS Corneas to Real Success —“Unaided” Vision! Crosslinking is often labeled a “success” when it halts the progression of Keratoconus, but what about the patient’s vision? Many are left with distorted optics, irregular corneas, and dependence on rigid contact lenses—struggling to function in daily life. So is stabilization without “Unaided” Sight truly […]
Correcting Extreme Keratoconus to 20/20 Vision with EVO ICL

Correcting Extreme Keratoconus to 20/20 with EVO ICL: A Visionary Breakthrough From Nigeria with Love: A Life Changed Forever Every day, patients from around the world arrive at Gulani Vision Institute, carrying the burden of impossible eye conditions—cases dismissed as untreatable by others. They leave with crystal-clear vision, and their heartfelt messages, gifts, and gratitude […]
A Valentine’s Day Miracle: From Advanced Keratoconus to 20/20 Vision

A Journey of Hope and Precision Valentine’s Day is a time for love, but this year, it’s also a celebration of vision, clarity, and life-changing transformation. Many people diagnosed with advanced keratoconus, irregular astigmatism, and polar cataracts are told that their only option is a corneal transplant. However, Maureen’s story proves that there is hope […]
ICL Surgery: Vision Correction Without LASIK

Vision correction has evolved far beyond traditional LASIK. For those who cannot undergo LASIK or prefer an alternative, ICL surgery (Implantable Collamer Lens) offers a safe, effective, and customizable solution. At Gulani Vision Institute, Dr. Arun Gulani has worked with ICL technology for over 3 decades including being certified in the most recent technological advancement […]
Can Keratoconus Be Cured?

Keratoconus, a progressive eye condition that causes the cornea to thin and bulge into a cone-like shape, often leads to distorted vision and frustration for patients. While many believe keratoconus is a lifelong challenge, Dr. Arun C. Gulani’s groundbreaking work offers hope for individuals seeking vision in more ways than one. Breaking the Myth: Keratoconus […]
Biggest Keratoconus Myth: Patients cannot lead a Full Life! WRONG!

Revolutionary Keratoconus Treatments at Gulani Vision Institute. Keratoconus, a progressive eye condition characterized by the thinning and bulging of the cornea into a cone-like shape, can significantly impact a patient’s vision and quality of life. Historically, patients with this condition have faced limitations in their daily activities, careers, and personal aspirations due to impaired vision. […]
Is LaZrplastique® Right for You? What Every Keratoconus Patient Should Know
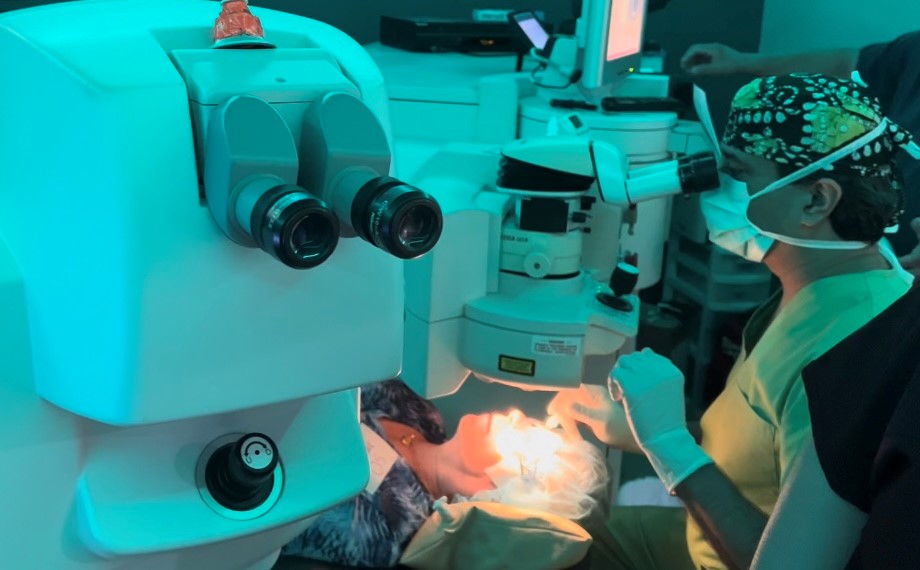
Living with keratoconus can be a challenging journey, but advancements in eye care have brought hope to millions worldwide. Among the groundbreaking treatments is LaZrplastique®, a next-generation, no-cut, no-flap laser vision correction technique pioneered by world-renowned eye surgeon Dr. Arun C. Gulani. Known for his innovative approach to vision correction, with over three decades of […]
